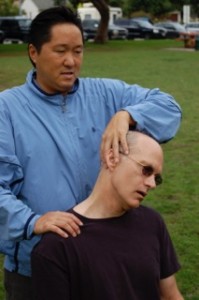
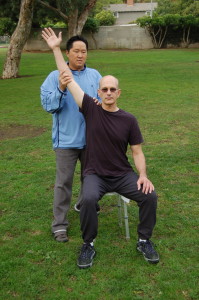
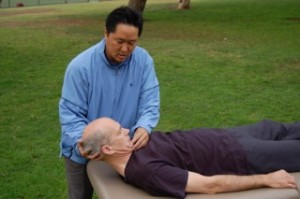
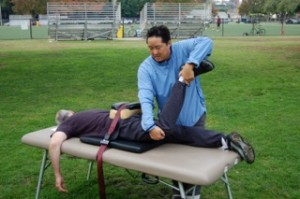
Sciatica nerve pain involves compression on the sciatic nerve. Sciatica nerve pain is closely related to chronic low back tightness in the L4, L5, S1 region. When the sciatic nerve is compressed, pain can be experienced anywhere along the pathway of the sciatic nerve. Nerve pain can occur anywhere down the leg to the foot or ankle. The source of sciatica nerve pain is from inflexibility in muscles that lie above the nerve. The primary area of compression comes from the pelvic region. In order to remove sciatic pain, the deep six muscles of the hip-thigh complex must be lengthened. The deep six muscles are also called the hip rotators. Elongating these muscles requires working with a stretching expert in Active Isolated Stretching technique. A skilled stretching coach can unwind the deep six muscles. These muscles are too deep inside the body to open through self-stretching methods.
Sciatica nerve pain causes are muscular inflexibility
Sciatica nerve pain involves numerous muscles being shortened which press on the sciatic nerve. The glutes, hamstrings, calves, ilio-tibial (I.T.) band, quadriceps, and psoas muscles all play a part in creating excessive pressure around the L4, L5, S1 region of the low back. Underneath all these major muscles are the deep six muscles, the hip rotators. The deep six muscles are: quadratus femoris, obturator externus, inferior gemellus, obturator internus, superior gemellus and piriformis muscles. The deep six muscles are located at the junction of the thigh and hip socket, six small muscles that control rotation of the hip deep within the hip socket.
The deep six
These deep six muscles are deep inside the pelvic region. The deep six muscles surround or lie just above the sciatic nerve. So when the hip rotator muscles become shortened, they press down and cause sciatic nerve pain. What causes these deep six muscles to get shortened? One way: when the larger muscles that lie above the deep six become shortened, they form a cast of tightness around the deep six muscles, forcing them to get tight.
Therefore, the way to unwind the deep six muscles is to first address all the muscles that lie above the hip rotators. I mentioned these muscles earlier: the glutes, hamstrings, I.T. band, psoas, etc. The other problem is that conventional stretching is inadequate at completely lengthening these target muscles. To do the job, we must use Active Isolated Stretching techniques which is fifteen times more effective than conventional stretching. Forget about PNF stretching, it has no way of approaching the deep six.
The goal in solving sciatica nerve pain is releasing all the muscles that impinge on the nerve pathway. The short answer is to release the hip rotators. But this cannot be done until the larger, more superficial (those that lie above) muscles are released first. Because sciatica nerve pain and L4, L5, S1 lumbar disc disease are closely related, releasing the deep six muscles will solve both problems simultaneously.
Sciatica treatment options. So many don’t work!
Sciatica is nerve pain. Nerve pain is caused by impingement. Impingement is caused by inflexibility in a series of muscles pressing down on the nerve. The way to solve sciatica nerve pain is to elongate all the inflexible muscles surrounding the low back. Surgery does not elongate muscles. Injections may reduce inflammation around the deep six muscles, but it doesn’t reduce inflammation around the muscles that surround the deep six. That is why epidural injections rarely provide a lasting solution. Deep tissue massage cannot reach the deep six muscles because they are underneath layers of dense muscles including gluteus maximus, gluteus medius, and the iliotibial band. Similarly, acupuncture needles cannot reach the deep six muscles because it is too deep. Active Isolated Stretching therapy has a different approach to solving sciatica pain than conventional treatment. AIS is simple in its approach, but detailed in its methodology. If you’ve had sciatica nerve pain for two, five or twenty years, and you’ve tried all the conventional treatments, now is the time to try Active Isolated Stretching treatment because it is an entirely different approach to solving a problem that perplexes other healthcare professionals.