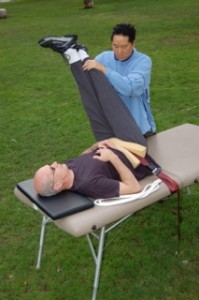
Migraine headaches and C5 C6 cervical disc disease commonly occur together. The commonality between migraine headaches and C5 C6 cervical disc disease is that tight muscles in the upper body and neck cause both problems. The migraine sufferer must address muscular tension in the neck to resolve migraine pain. Another critical area that causes migraines is the jaw muscle, the digastric. Migraine therapy involves treating the jaw, the neck, and the upper body. One tried approach has been seeking long term chiropractic treatment in the hope that regular adjustments would dismiss the herniation (or degeneration) in the C5, C6 region and solve migraine pain at the same time. The new migraine headache specialist is trained in Active Isolated Stretching.
Migraine headaches and C5 C6 problems are caused by excessive muscular tension
Migraine headaches and C5 C6 cervical disc abnormalities are both affected by inflexibility in numerous upper body muscles. Tightness in the neck muscles – the scalenes, the sternocleidomastoid, the levator scapula, creates excessive stress on the cervical discs. This excessive pressure causes the discs to herniate or degenerate. Furthermore, cervical disc disease is caused by more than just tight neck muscles, it also involves tightness in the chest, upper arms, shoulders, and upper back muscles. These areas are the base on which the neck rests. If the base is abnormally tight, then the neck muscles cannot unwind.
All the above mentioned muscular areas affect migraine headaches too. When the upper body is tight, and the neck muscles are tight, these muscles will pull on the skull. Muscles of the neck attach at the skull and the shoulder. This pulling strain causes migraine headaches. The trapezius muscle is one of the prime bandits that pulls on the base of the skull, the occiput.
The jaw: a source of migraine headache pain
The other essential area in migraine pain are the muscles of the jaw. Migraine pain will not be solved until the digastric jaw muscle is relaxed. Cranial nerves pass under the digastric. When the digastric muscle gets tight, it can press into the cranial nerves which induces pain signals to the head. Tightness in the jaw is connected to muscular inflexibility in the upper body and neck muscles. Active Isolated Stretching therapy focuses on the numerous muscles causing migraines. Muscles work in groups. An advanced practitioner of Active Isolated Stretching is a migraine headache specialist.
Treating migraines and treating C5, C6 cervical disc disease is part of the same process. What helps migraines will also help C5, C6 issues. People who suffer from migraines headaches and C5 C6 issues are also affected by cervical neck issues. However, not all people with C5, C6 deterioration will experience migraine headaches.
Other treatment options for migraines
Chiropractors have suggested that adjustments will cure C5, C6 abnormalities; That the source of migraine headaches and C5 C6 disc disease may result from a subluxation. Unfortunately, chiropractic has not linked the relationship between subluxation and muscle tightness. Chiropractic and AIS can work well together. If migraine sufferers have tried chiropractic alone and are still in pain, then the new approach is Active Isolated Stretching which skillfully releases overly tense upper body muscles; getting to the root cause of migraine headaches and C5 C6 cervical disc disease. Some will supplement AIS treatment with chiropractic adjustments. If they do, the chiropractic adjustments will be more productive after Active Isolated Stretching (AIS first, then chiropractic). Others will decide not to follow-up AIS with chiropractic. Either way, Active Isolated Stretching will be effective at resolving migraine headaches and C5 C6 issues.
How can something so simple as stretching solve migraine headaches?
It is important to note that Active Isolated Stretching is not to be confused with ordinary stretching. AIS is capable of producing lasting changes to myofascial pain syndromes. Migraine headaches are a myofascial pain syndrome. This means that the cause of migraine headaches are related to the muscles and the fascia (connective tissue that surround and weave through the muscles). In the case of migraines, the area of focus is the upper body. AIS treatment focuses on opening the chest, upper back, neck, and jaw muscles to resolve migraine head pain. If you are a migraine sufferer, ask yourself if these areas are overly tight? The approach is comprehensive but simple.
Distinguishing marks of Active Isolated Stretching
Distinguishing marks of AIS are: 1.)You can not open the neck muscles until you open the chest, shoulder, and upper back muscles. 2.) A target muscle (particularly a tw0-jointed muscle) must be opened at six points to completely open it. No other form of stretching advocates either of these two theories which is why ordinary stretching has been unable to resolve migraine headaches and C5 C6 cervical disc herniation or degeneration.
AIS practitioners that treat migraine headaches are a small group
The number of advanced AIS practitioners who can competently handle migraines is small. Maybe fifty. Those suffering from migraines will typically go any distance to be treated by a good migraine headache specialist. Travel may be necessary. Expect session length to be multiple hours. After one or two sessions, the sufferer will notice productive changes.